INFORMATION FOR MEMBERS OF THE GENERAL
PUBLIC TO HELP PROTECT AGAINST Q FEVER
What is Q fever?
Q fever is an infectious disease spread to humans by animals and caused by the bacterium Coxiella burnetii. The bacterium is…
How does Q fever spread?
Q fever is mainly spread from animals to humans via inhalation of infected particles in the air. Other routes…
Q fever Symptoms – Acute and Chronic
Once exposed to the bacterium Coxiella burnetii, people may react to the infection in different ways. Following infection by…
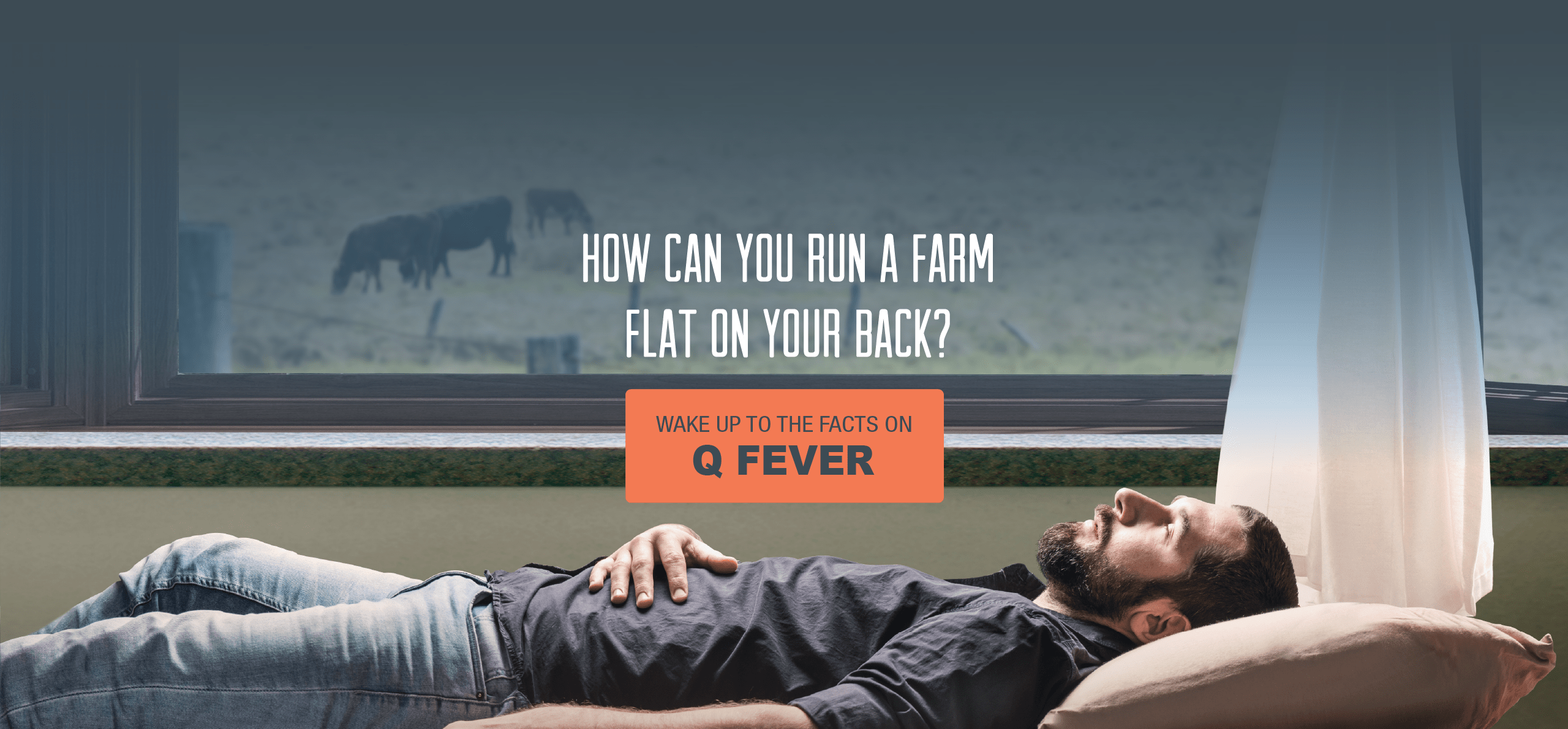
Who is at risk of Q fever?
People at increased risk of contracting Q fever include those in direct contact or in close proximity to infected animals…
How can you help prevent Q fever?
It is important to implement control measures to minimise the spread of Coxiella burnetii from…
Get medical advice on your Q fever risk
Any medical practitioner can provide Q fever advice. The benefit of visiting your regular doctor is that they get…