In Australia, any case of Q fever needs to be reported to health authorities. Please see your doctor if you think you have symptoms of Q fever.
Acute Q fever
Acute Q fever symptoms may include:
- Fever that starts abruptly and can last several weeks
- Chills
- Sweating
- Severe headache
- Aching muscles and joints
- Extreme tiredness and confusion
- Nausea and diarrhoea
- Blurred vision or extreme sensitivity to light
- Weight loss
- Rash
Typical symptoms of acute Q fever appear 2-4 weeks after infection and in most cases disappear without treatment. Symptoms can last up to 3-6 weeks.
Click to learn about Jason’s experience with acute Q fever
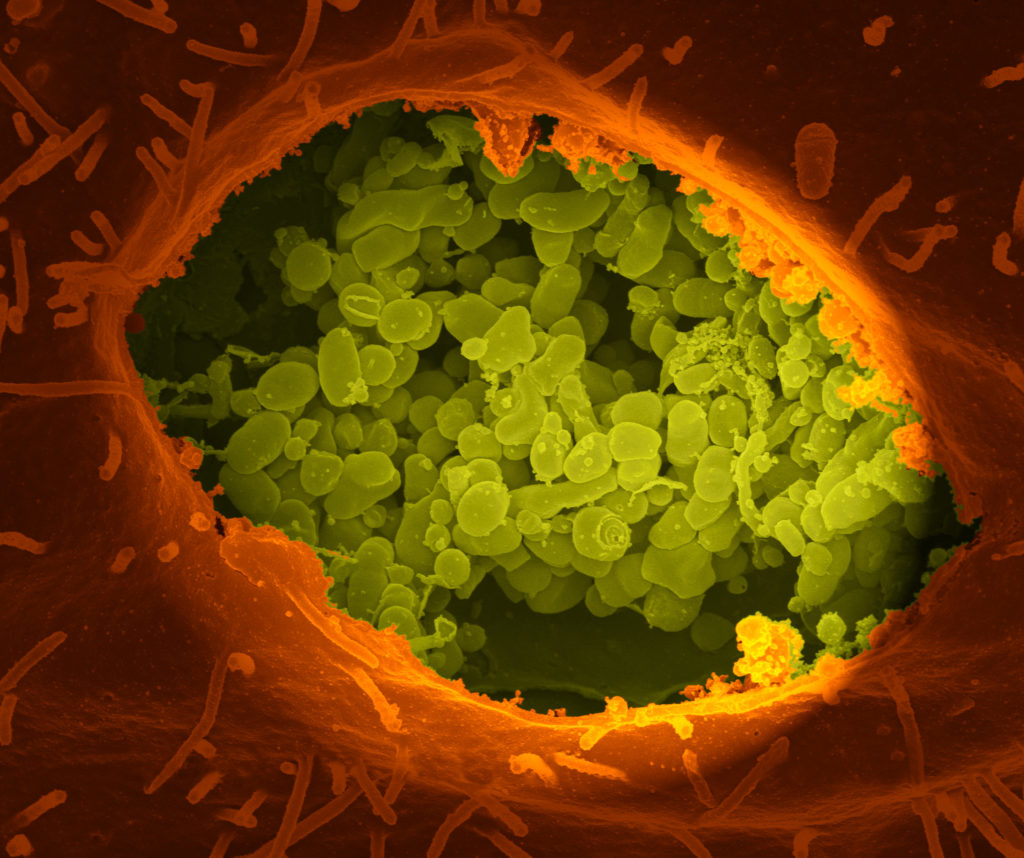
Chronic Q fever
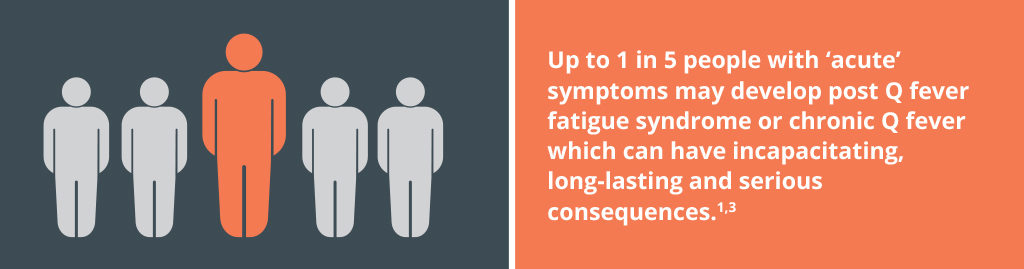
Chronic Q fever is a serious and long-lasting disease and occurs in up to 5% of acute Q fever patients.3 It results from persistent infection in one or more parts of the body. It may develop months or even years after the initial episode of Q fever, even in patients that did not have any symptoms to start with and may take years to resolve. A common manifestation of chronic Q fever infection is inflammation of the heart (endocarditis), which more commonly develops in people with certain heart problems. However, individuals may also suffer from persistent infections occurring in the liver, bones and other organs.
Click to learn about Geoff’s experience with chronic Q fever & post Q fever fatigue syndrome
Post Q fever fatigue syndrome
Some patients with acute Q fever (up to about 15%) will go on to experience a post-Q fever fatigue syndrome, where symptoms continue to persist for more than 12 months after symptoms first appear.1,2 Symptoms associated with post-Q fever fatigue syndrome (extreme tiredness and other symptoms), can last for years and have the potential to be highly incapacitating.
Click to learn about Geoff’s experience with chronic Q fever & post Q fever fatigue syndrome